In the evolving field of surgical oncology, the trend has shifted increasingly toward minimally invasive interventions. While traditional surgery remains a cornerstone of treatment, there are many instances where a patient may not be a candidate for major surgery, or where the tumor is located in a position that makes resection difficult. This is where CANCER Ablation Therapy provides a vital alternative. Ablation therapy refers to a group of procedures that use extreme heat, cold, or chemical agents to destroy cancer cells directly within the body without the need for large incisions. This targeted approach allows for the destruction of malignant tissue while preserving the function of the surrounding healthy organ.
The Science of Localized Destruction
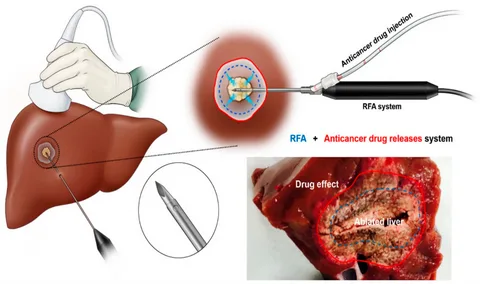
The fundamental goal of ablation is “in situ” tumor destruction. Unlike systemic treatments like chemotherapy, which circulate throughout the entire body, ablation is a localized treatment. It is most commonly used for tumors in the liver, lungs, kidneys, and bone. The procedure is typically performed by interventional radiologists who use advanced imaging technology to guide a needle-like probe through the skin and directly into the tumor.
The choice of ablation method depends on the size, location, and type of the tumor. The most frequently utilized techniques include:
-
Radiofrequency Ablation (RFA)
RFA is perhaps the most widely used thermal ablation technique. It utilizes high-energy radio waves to generate heat. A thin probe is inserted into the tumor under the guidance of ultrasound or CT scans. Once in place, an electric current is passed through the probe, creating heat that “cooks” the cancer cells, leading to coagulative necrosis.
-
Microwave Ablation (MWA)
Similar to RFA, MWA uses electromagnetic waves to generate heat. However, MWA can reach higher temperatures more quickly and is often more effective for larger tumors or those located near blood vessels. Because blood flow can act as a “heat sink” (cooling the area and protecting cancer cells), the rapid, intense heat of MWA is often preferred in highly vascularized organs like the liver.
-
Cryoablation (Cryotherapy)
While RFA and MWA use heat, cryoablation uses extreme cold to destroy tissue. A specialized probe, called a cryoprobe, is inserted into the tumor, and argon gas is circulated through it to create an “ice ball” that encompasses the malignancy. The cycle of freezing and thawing ruptures the cell membranes and destroys the tumor’s blood supply. This technique is often favored for kidney tumors because it preserves the structural integrity of the surrounding collecting system better than heat-based methods.
-
Irreversible Electroporation (IRE)
IRE, often referred to by the brand name NanoKnife, is a non-thermal ablation technique. It uses short, high-voltage electrical pulses to create permanent “pores” in the cell membranes, causing the cells to die. Because it does not rely on heat or cold, it is particularly useful for tumors located very close to vital structures like major nerves or bile ducts, which could be damaged by thermal energy.
Clinical Applications and Patient Selection
Ablation therapy is not a universal replacement for surgery, but it is an essential tool in a multidisciplinary oncology strategy, such as those implemented atLiv Hospital. It is particularly effective for:
- Small Primary Tumors: For patients with early-stage lung or kidney cancer who have limited lung or kidney function, ablation can offer a curative-intent treatment with minimal risk.
- Metastatic Disease: Patients with a limited number of metastases in the liver (often from colorectal cancer) or lungs may undergo ablation to control the spread of the disease.
- Palliative Care: In cases where a cure is not possible, ablation can be used to shrink tumors that are causing pain or obstructing vital pathways, such as in bone metastases.
The success of the procedure is highly dependent on the “surgical margin”—ensuring that the zone of destruction extends slightly beyond the visible edges of the tumor to catch any microscopic spread.
Advantages and Recovery
The primary advantage of ablation therapy is its minimally invasive nature. Most procedures are performed under conscious sedation or general anesthesia, and because the entry point is only a small needle puncture, the physical trauma to the body is significantly reduced.
Patients typically experience:
- Shorter Hospital Stays: Many ablation procedures are performed on an outpatient basis or require only an overnight stay for observation.
- Reduced Pain: Compared to open or even laparoscopic surgery, postoperative pain is generally mild and easily managed with over-the-counter medications.
- Lower Complication Rates: There is a lower risk of infection and bleeding compared to traditional surgical resection.
- Repeatability: If a new tumor appears or if the original tumor is not completely destroyed, ablation can often be repeated safely.
Monitoring and Follow-Up
Post-procedural care involves rigorous imaging follow-up. A CT or MRI scan is usually performed a few weeks after the ablation to confirm that the entire tumor has been treated. On these scans, the treated area appears as a “dead zone” without any blood flow. Over time, the body’s immune system cleans up the dead tissue, often leaving only a small scar. If any enhancement (blood flow) is seen at the edges of the ablation zone, it may indicate residual cancer, necessitating further treatment.
The transition from clinical intervention to long-term health is a vital phase of the patient journey. While medical teams focus on the technical destruction of the disease, the patient must focus on rebuilding the body’s natural defenses. Adopting a holistic view of recovery—one that prioritizes anti-inflammatory nutrition, mental clarity, and restorative movement—is essential. By finding balance and learning tolive and feel more attuned to their physical and emotional needs, survivors can maximize the benefits of their medical treatments and move toward a future of sustained vitality.